
In celebration of National Donate Life Month this April, GMHC had a flag-raising ceremony on April 10th. The act symbolizes our collective appreciation for the miracles of organ, eye and tissue donation and recognizes those who have chosen to give the invaluable gift of life. During the event, two donor stories were shared. One from a living donor, Jody Wille, and one from a recipient, Donna Simon.
In 2023, Iowa stood as a beacon of hope and generosity. 123 organ donors provided 350 organs for transplantation, offering a second chance at life for many. Additionally, 1,027 tissue donors from our state brought healing and relief to countless individuals, three of which came from GMHC, each tissue donor impacting 50 to 350 people’s lives. Despite these life-changing acts, over 106,000 people in the U.S. are still waiting for a crucial organ transplant, including more than 600 Iowans.
The Donate Life flag raising ceremony not only highlights the ongoing need for life-saving transplants but also salutes the donors and families for their profound act of giving. Every donor has a story, and each story is a testament to human kindness and resilience.
Jody Wille
Jody Wille’s uncle, Owen Harbaugh, had kidney damage due to hypertension. When his kidneys stopped functioning, he had to go on dialysis for a short period of time. That is, until his niece, Jody Wille, who was a perfect match, stepped up to donate one of her kidneys.
Owen was a veteran and in August, 2002, surgeons from UIHC came to the VA in Iowa City to perform the 3 to 4 hour surgery. Surgery was on a Thursday. Jody was out of the hospital by Saturday while her Uncle Owen stayed a few more days to ensure his body was adjusting to Jody’s kidney. And, it did!
“The surgeons told them that most kidneys sleep a while before working in the new recipient, but mine started working right away in Uncle Owen,” said Jody.
“My uncle was very close to our family and I felt this was the least I could do for him. Uncle Owen was never married or had children, so my siblings and I were like his kids,” said Jody.
“I tell people that being a living donor is giving a gift that keeps giving, not only to the recipient, but to their family and friends who get to spend more time together. Uncle Owen lived with my donated kidney for 18 more years, attending family celebrations like weddings and graduations of his numerous nieces and nephews, and birthday parties of his beloved great nieces and nephews.”
Although Jody was told that the surgery is harder on the person who donates than the person who receives, that was not true for her. She exercised daily prior to surgery by walking 3-5 miles per day and drank plenty of water. Jody was off work for about four weeks for her recovery, and declared, “It was well worth it for our family to have those extra 18 years with Uncle Owen.”
Donna Simon
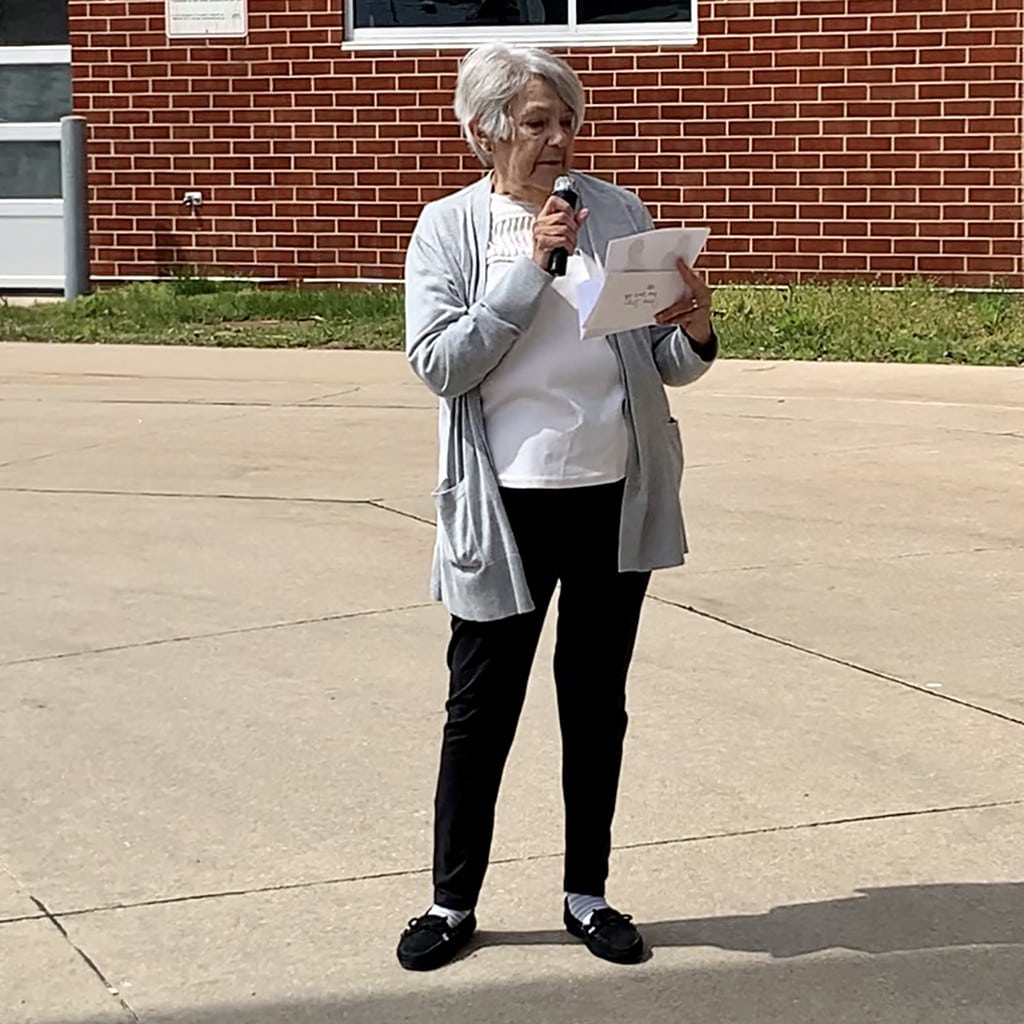
Donna Simon, a double lung recipient, was present to read a heartfelt letter that was written and sent to her by the mother of Donna’s 21-year-old donor. The letter described how he was a musician, enjoyed football and wrestling, left behind a son, and how he had a big heart. “He was a hero and signed up just in case something ever happened to him,” the letter read. The letter also included photos of the young man and his son. Donna shared the change that this gift has made in her life, allowing her to be more active with her children and grandchildren, and at the ceremony without her oxygen port.
The trend of hope continues to rise in Iowa, with increasing numbers embracing organ and tissue donation. You too can be a part of this journey of hope and healing. Register at IowaDonorNetwork.org to be a registered donor and join GMHC on Friday, April 12th by wearing blue or green to build awareness for donating life.








